Government assistance programs were expanded during the pandemic in extraordinary ways – those expansions that served vulnerable communities are now expiring.
The Families First Coronavirus Response Act (FFCRA) required the continuous enrollment of Medicaid beneficiaries in an effort to ensure millions of Americans had access to health care. With the expiration of the COVID-19 public health emergency (PHE) looming, states are beginning the unwinding of Medicaid continuous enrollment, which is anticipated to bring unprecedented challenges to states, safety-net providers, and Medicaid beneficiaries.
Of primary concern are the estimated 15 million people at risk of losing access to Medicaid health coverage when the PHE and continuous enrollment ends.
While it’s uncertain the exact number who will be disenrolled during the unwinding process, millions will likely lose coverage as their eligibility is redetermined. The process to redetermine eligibility for millions seeking Medicaid coverage in a short period of time presents significant administrative challenges for state agencies and safety-net providers.
States have an opportunity to mitigate the impact to agencies, safety-net providers, and beneficiaries by taking proactive and strategic action through data insights and outreach.
Overview of Medicaid
As the nation’s public health insurance program, Medicaid provides health coverage to nearly 1 in 5 Americans, including close to 39 million children, 18 million low-income adults, and 8 million elderly and disabled individuals. While enrollment differs by state, over half of Medicaid recipients are under the age of 21. Eligibility criteria to enroll in Medicaid is predicated on several factors, but is usually tied to a higher need for health care whether caused by disability, age, pregnancy or a chronic condition.
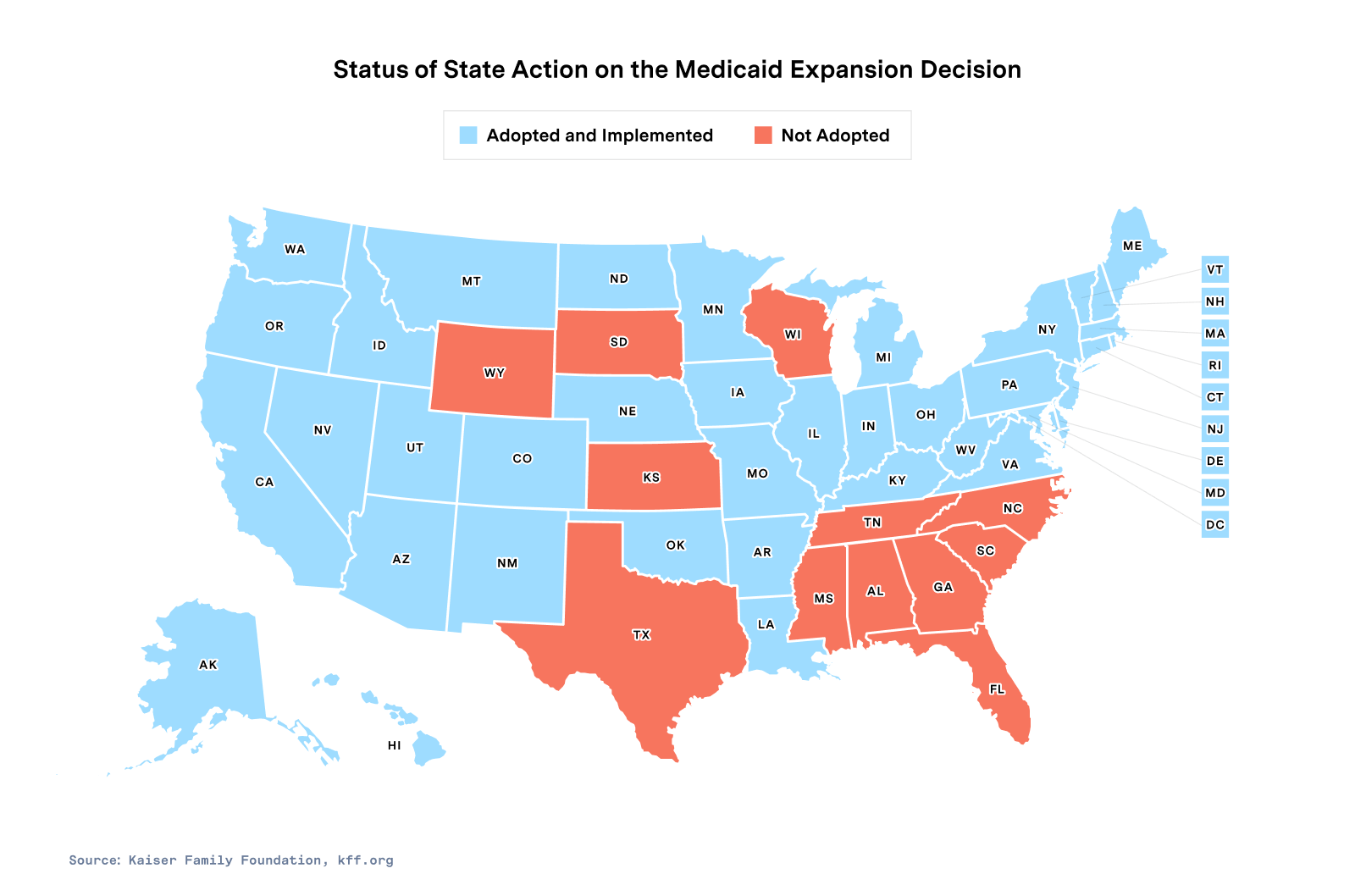
Federal eligibility criteria for Medicaid expanded in 2010 with the passing of the Affordable Care Act (ACA), with enhanced federal matching funds to states offering expanded coverage. The expansion has helped provide healthcare to low-income adults without dependent children in all states, except 12 that chose not to expand Medicaid under the ACA.
How COVID changed enrollment and eligibility
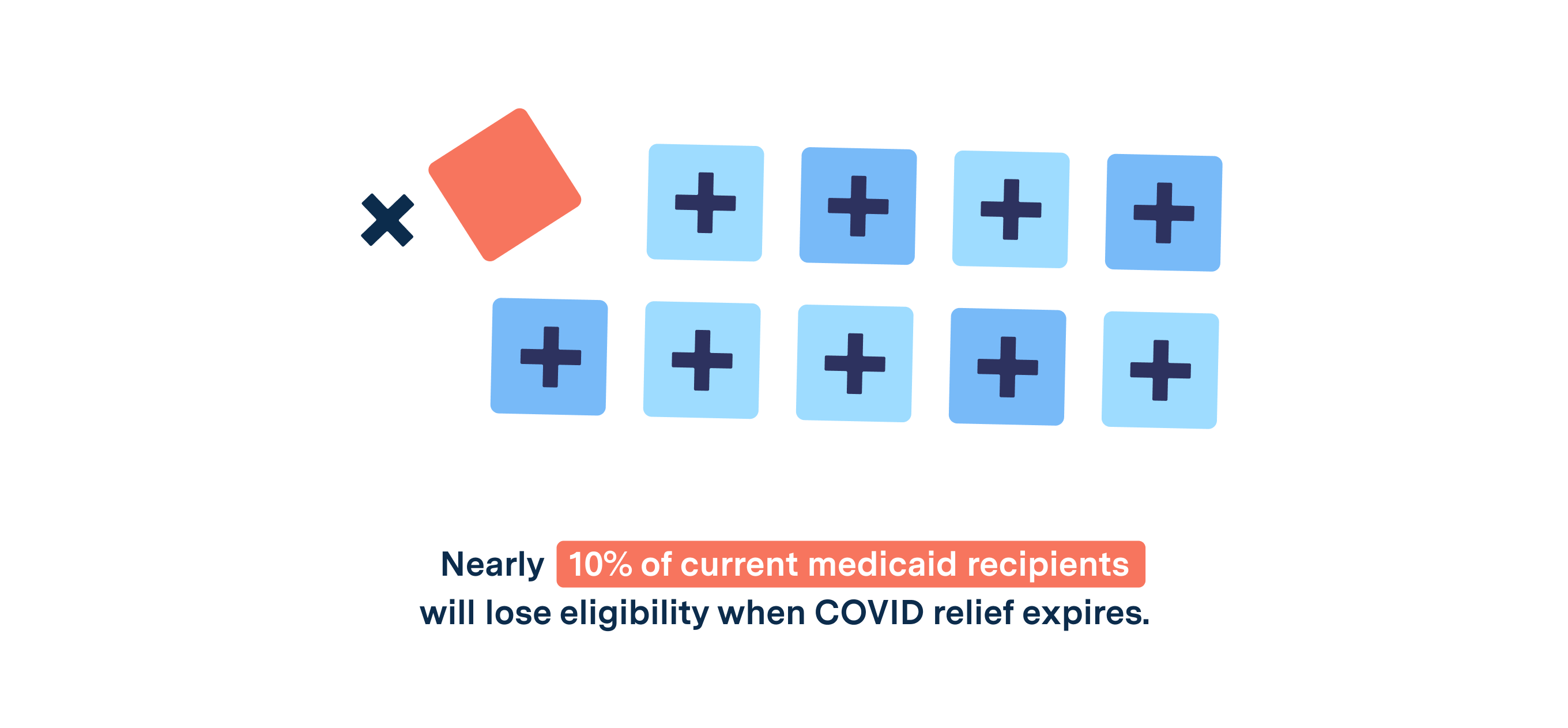
During the pandemic, Medicaid enrollment increased by nearly 25%, or 22.2 million people, increasing the total number of Medicaid beneficiaries to 89 million. All states saw an increase in Medicaid and CHIP enrollment, with some by as much as 70%.
The increase in Medicaid enrollment over the past two years is largely attributed to the continuous enrollment requirement and the lack of churning, or the temporary loss of coverage as people disenroll and re-enroll. Other factors for increased enrollment include changes in the economy, inflation and rising housing costs that have placed more people in positions of need.
What is clear is that continuous coverage has long term positive effects on the individuals enrolled, including improved health and financial stability, as well as overall community strength and the lowering of total costs.
The Medicaid unwinding process
As continuous enrollment ends, those most at risk of losing coverage are low-income adults in states that have not opted-in to Medicaid expansion. Those affected disproportionately live in underserved communities and are more likely to be in additional assistance programs.
Safety-net providers are concerned patients will lose membership to managed care plans as a result of Medicaid unwinding, which will lead to patients forgoing treatment for chronic conditions or specialized care for cardiac, mental health and addiction issues.
Other recipients are at risk of losing coverage because they may not have received renewal notices from the state if they relocated during the pandemic. It’s been estimated that over 11% of Americans relocated during the pandemic due to financial hardships, evictions, or lack of affordable housing.
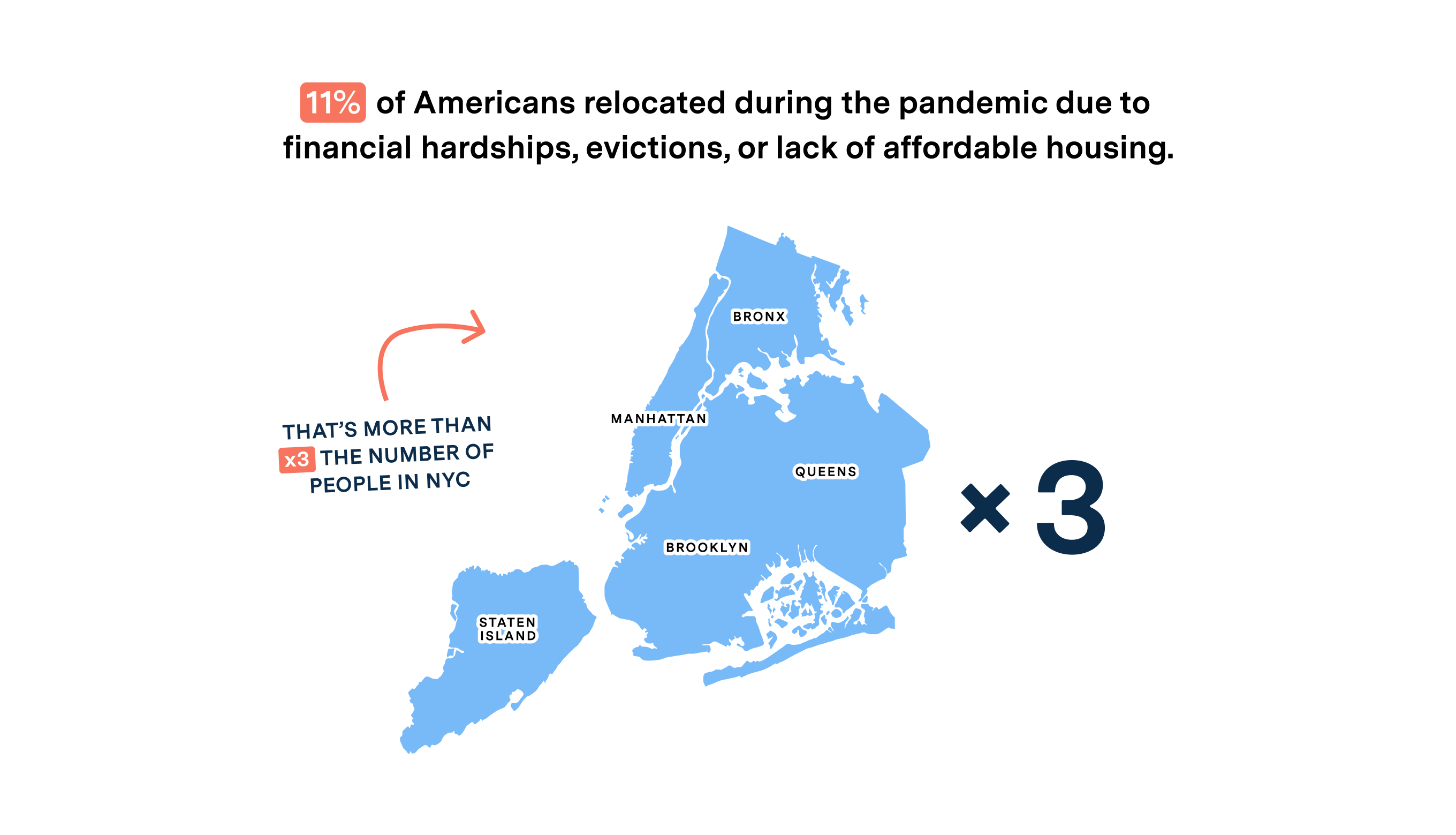
Most who relocated are low-income, disabled, or elderly. Administrative challenges related to re-enrollment may also impact those with limited English proficiency. These groups are also likely to be enrolled in additional government assistance programs, such as SNAP. When they do not receive these services, the negative effects reverberate in their new communities, causing broader instability.
How technology and data can identify coverage gaps
The stakes of Medicaid unwinding are high, the least of which are the economic impacts of 15 million people losing health care coverage. Not only will health care providers, community health centers, and other safety-net providers be strained to support high-risk patients, providers will also lose a large source of revenue if patients lose insurance.
Since Congress passed the FFCRA and increased the federal Medicaid match rate (FMAP) in early 2020, states have received approximately $100.4 billion from the Federal government to support Medicaid continuous enrollment. That is money injected into local communities that will be felt if it goes away.
Studies examining the fiscal impacts of Medicaid continuous enrollment on state budgets show that fiscal relief provided by enhanced FMAP was more than double the state costs of additional Medicaid enrollment during the pandemic.
While state Medicaid spending was low during the pandemic, state spending should begin to increase as FMAP funding subsides, despite the expected reduction in Medicaid enrollment. Without a complete picture of the changes that have occurred over the past two years, and with a complex process to navigate on the horizon, states will need access to timely data to accurately monitor and report on unwinding progress.
To manage the complexity and assess Medicaid unwinding progress, states are required to track a set of baseline metrics set by the Centers for Medicare and Medicaid Services (CMS). But states should consider paying attention to additional metrics in order to analyze the long-term impact of unwinding.
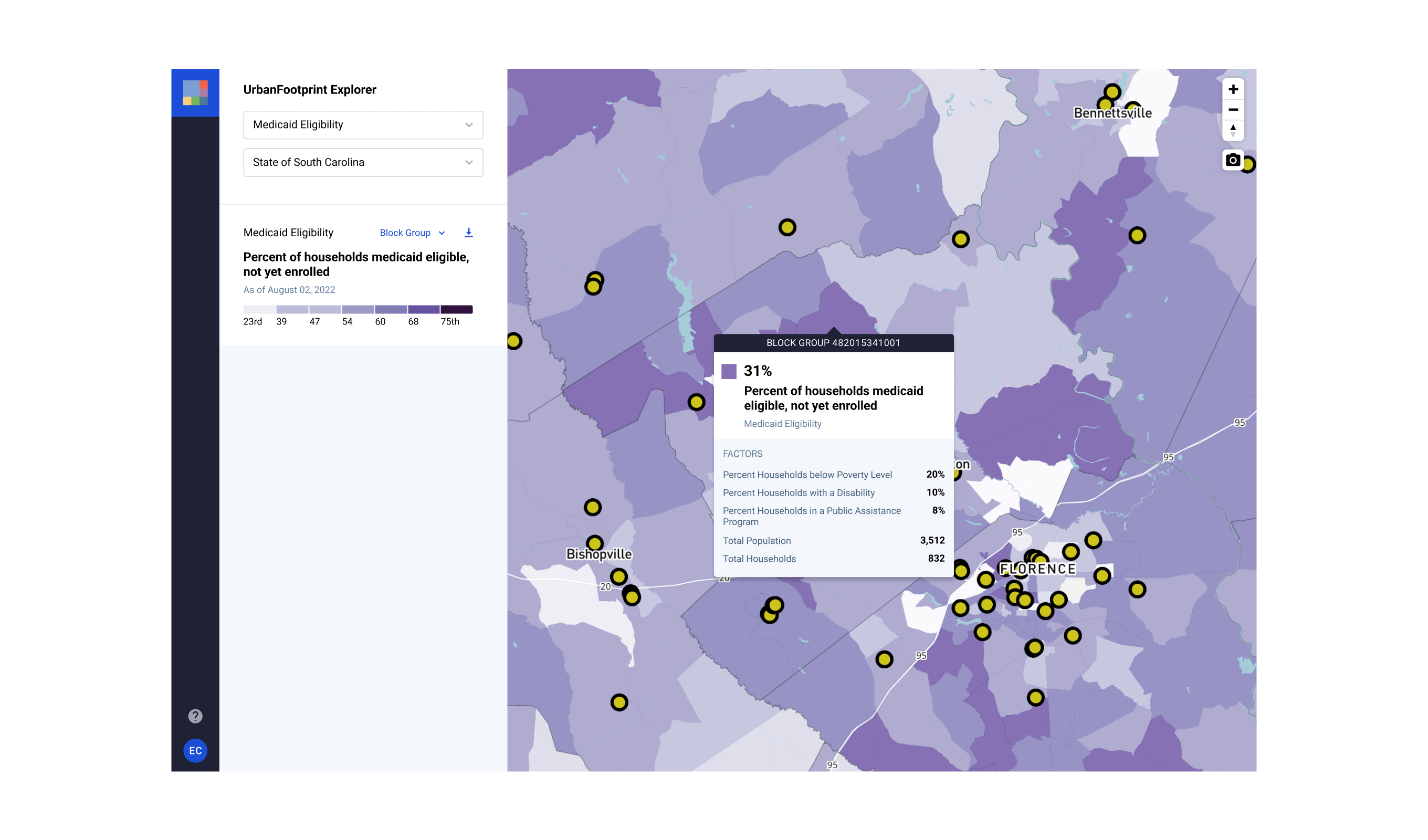
Leveraging insights into areas of high-risk, gaps in safety-net providers, and the locations of eligible populations, state agencies will be able to more effectively target outreach, improve unwinding performance, manage state Medicaid funding, and meet program reporting requirements.
We must act before it’s too late
Taking a proactive, targeted approach to Medicaid unwinding will not only save money, but also reduce the impact on millions of Americans. Using location and demographic data insights to target at-risk populations is a must. The stakes of Medicaid unwinding are high, but with the right technology and access to data insights, states can have a clear picture of changing eligibility and enrollment to ensure consistent coverage for their most vulnerable populations.